
Briana Martin, MSPE
Research & Evaluation Associate

Amy Willa, MPH
Research & Evaluation Associate

Shao-Chee Sim, PhD, MPA
Executive Vice President for Health Policy, Research & Strategic Partnerships
High-quality primary care is essential to building and sustaining a healthy population. As a foundational component for healthy communities, primary care deserves continued attention, support, and development to ensure access to all.
In Texas, however, we face an unfortunate truth: Many Texas adults don’t have a primary care provider.
Primary Care Provider access in Texas
Health care access and affordability is a complex and ongoing issue often connected to one’s insurance status and . New data show that these non-medical drivers of health (NMDOH) reinforce disparate access to healthcare among Texans.
In partnership with SSRS, the Episcopal Health Foundation (EHF) conducts annual, statewide polls to understand Texans’ views on state health policy priorities and their experiences with health care accessibility and affordability. Since 2018, we have observed interesting trends in Texans’ usual source of care. Although primary care is a critical element in one’s health care journey, nearly one-third of Texans do not have a usual place of care (27% in 2018 and 29% in 2021).
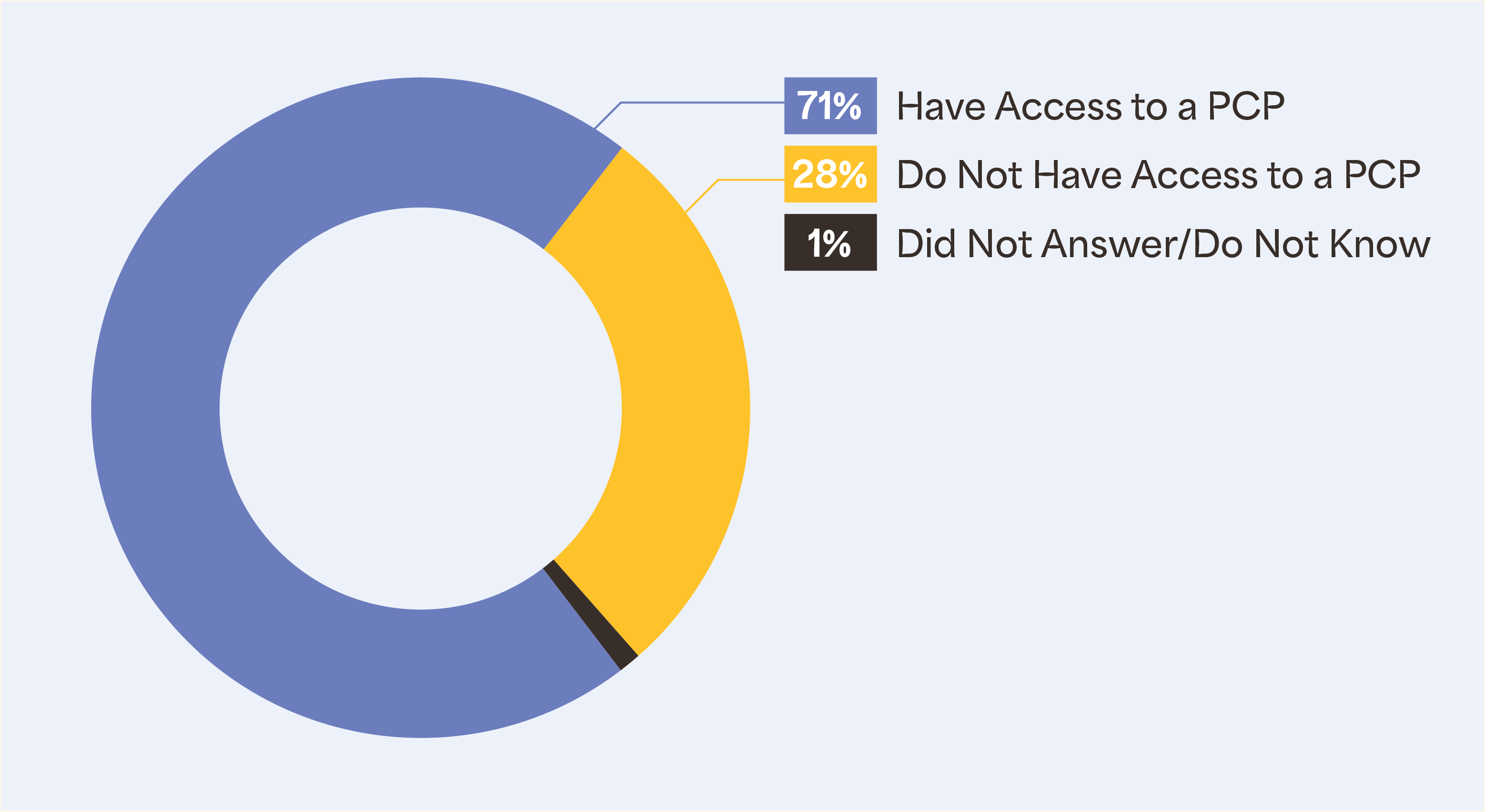
Understanding that primary care is a critical element in a person’s health care journey, it is necessary to acknowledge, address, and erode the barriers to access a primary care provider (PCP). In 2022, EHF introduced a survey question to inquire about PCP access among Texans. And the results are astounding.
28% of respondents do not have a primary care doctor or a provider they visit for regular check-ups, when they are sick, or when they need advice about their health. Of those who do not have access to a PCP, most are Hispanic, compared to other races/ethnicities. Additionally, when comparing educational access, poll results show that Texans with a high school diploma or less fare worse in PCP accessibility.
View Figure 2 below to see a breakdown of PCP access in Texas by race/ethnicity, education, and poverty.
Health care affordability and income influence PCP Access
The relationship between health care affordability, income, and PCP access reveals PCP access as a more complicated and dynamic process than previously demonstrated.
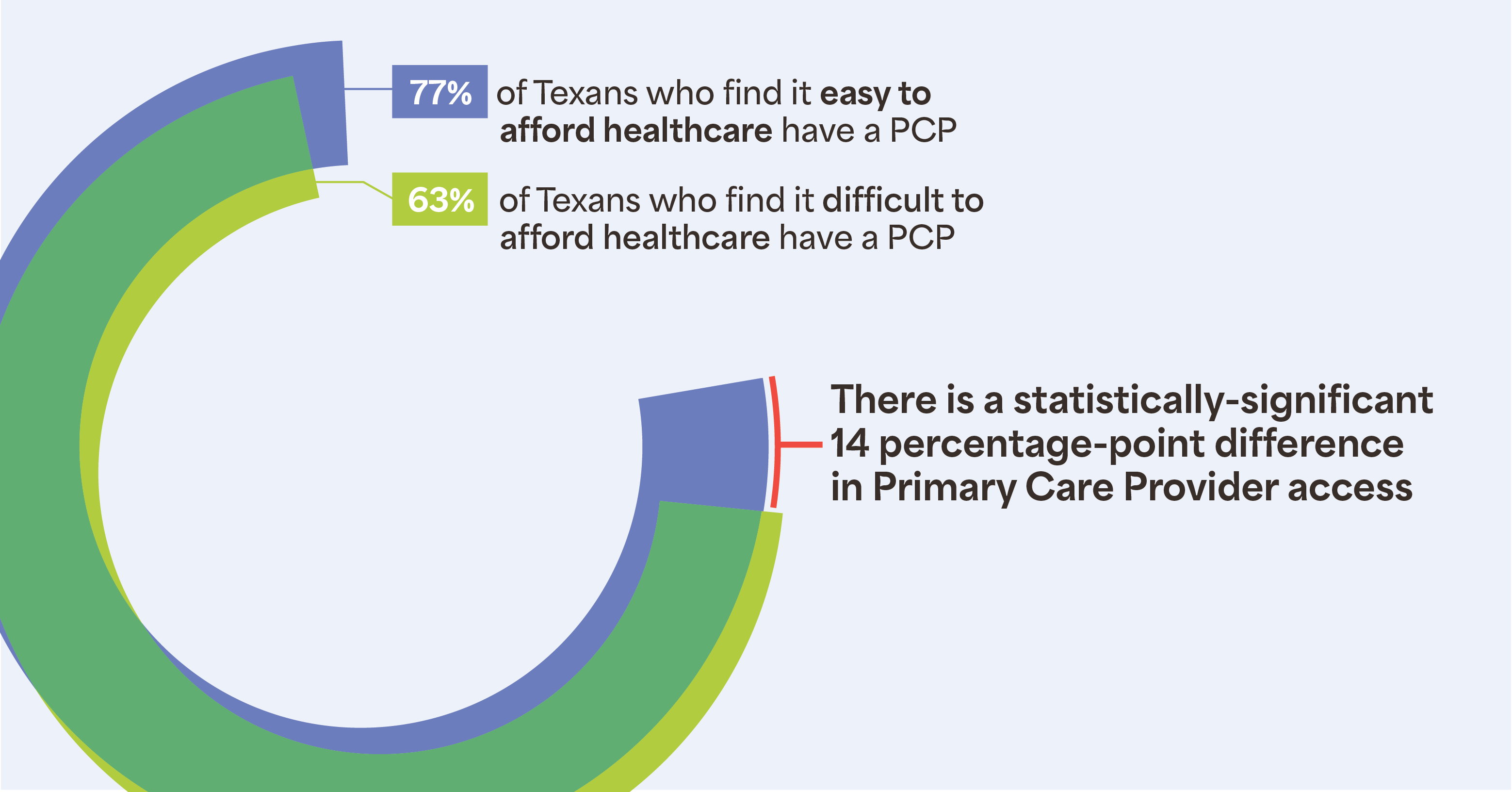
Two significant findings rose to the top:
- 77% of those who find it easy to afford health care report having a PCP compared with those who find it difficult to afford care, of which only 63% report having a PCP (see figure 3).
- 82% of those with household incomes more than 250% of the federal poverty level (FPL) report having a PCP compared to 62% of those with incomes less than 250% FPL.
Simply put, individuals who find it difficult to afford health care and those who have less income are less likely to have a PCP compared with individuals for whom affording health care is easy and who have higher income.
Reports show that nationally, uninsured rates reached an all-time low in 2022; however, Texas remains the uninsured capital of the United States. Health care coverage can influence whether people get the necessary preventative and medical care that they need, especially if they don’t have a usual place of care. Without advancements in health care affordability, access to primary care and its’ benefits for uninsured Texans will continue to lack.
Our survey findings also show the broader relationship between income inequality and health outcomes. Results from our 2021 survey show that Texas adults without health insurance are skipping/postponing care and experiencing problems paying medical bills at a high percentage.
Circumstances such as these can contribute to difficult realities. For example, someone not going to a primary care provider for usual care may not receive needed preventative care, making it much harder to detect risk factors for chronic illness and preclude preventable health decline. Additionally, struggling to pay medical bills can increase medical debt, reinforcing the enormous wealth gap in this country. Patterns like these illustrate how one’s socioeconomic status is a major non-medical driver of their health. With the well-being of Texans at stake, developing sustainable solutions for ensuring PCPs are accessible to all Texans requires focused policy priorities.
Primary care in Texas policy
The state of primary care and PCP access warrants continued attention and commitment to creating policies to address these realities.
Attention to primary care can appear in several ways during policy conversations. The Texas Primary Care Consortium (TPCC) includes simplifying signups and renewals and increasing provider reimbursements as potential policy areas of focus for increasing access to care.
Fortunately, the 88th legislative session allowed for several primary care policy wins to advance access to primary care in Texas. Of those, a notable win is the passing of HB12, which increases pregnant women’s Medicaid coverage from 60-days to twelve months post-partum. This advancement gratefully expands primary care access and supports healthy moms in Texas. Maternal health is a national priority as data continues to reveal the maternal mortality crisis in the U.S., the outcomes of which are the worst out of all high-income countries. Expanding health care access can be the impetus Texas needs to address the stark, disparate, and sometimes fatal, circumstances facing pregnant women.
These recent achievements are evidence that the idea of advancing primary care through policy has reached some ears, minds, and hearts. Hopefully, attention and support for essential bills like these will garner momentum for achieving greater things across the state.
Though we have experienced recent policy wins in Texas, competing forces may still threaten primary care. Texans’ PCP access may be further implicated by the sunset of the federal public health emergency (PHE) and the inherent insurance coverage benefits. Notably, the Georgetown University McCourt School of Public Policy released data showing over 1.3 million Texans being removed from Medicaid with a large percentage terminated for “procedural reasons.”
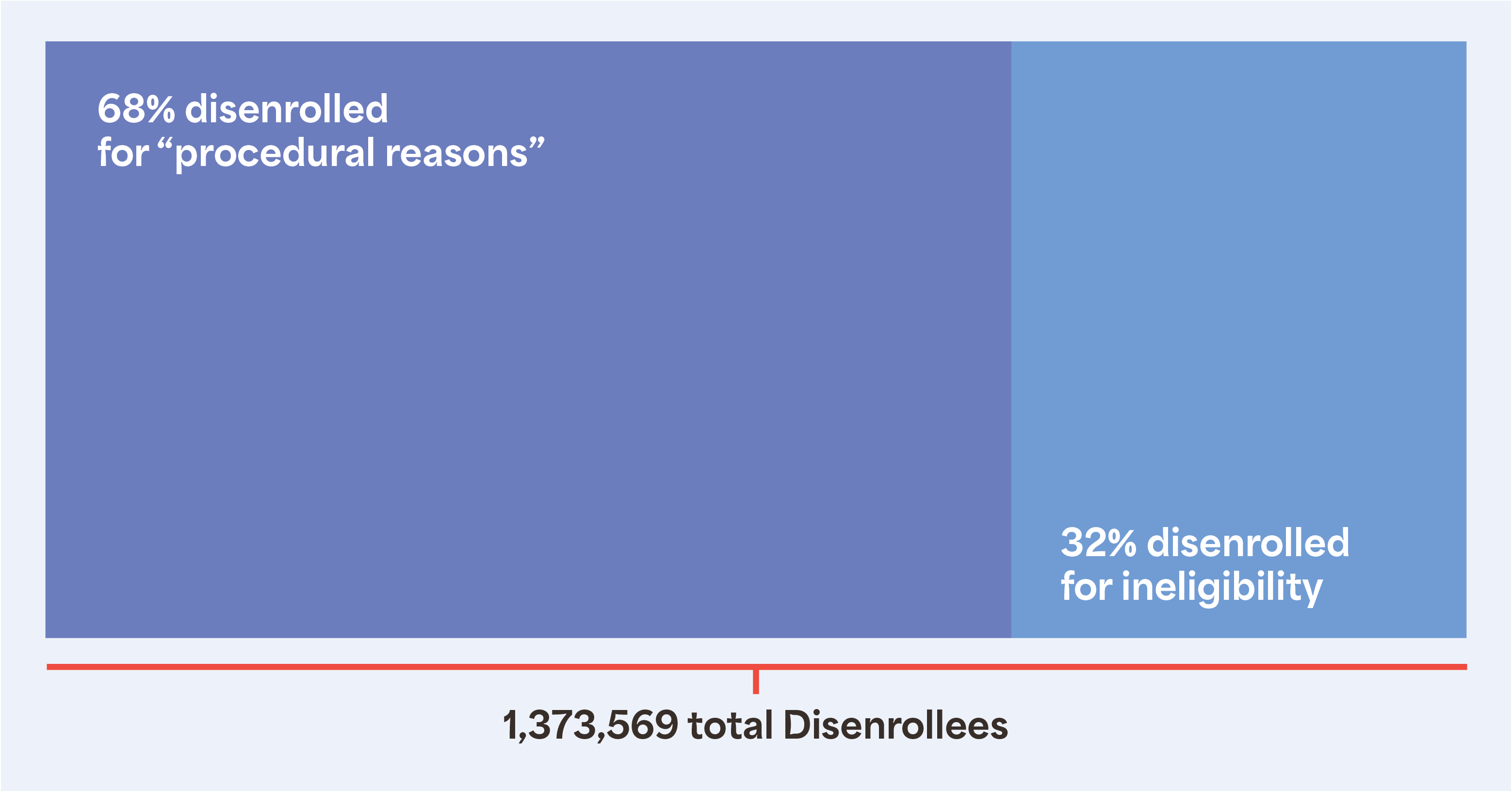
The realities of the unwinding process support the ongoing plight for Medicaid expansion in Texas. People have not only lost insurance coverage that they may still be eligible for, but they may no longer have access to the consistent care that they had for over two years. Unfortunately, potential progress on their health and wellness journeys may be stunted for the foreseeable future.
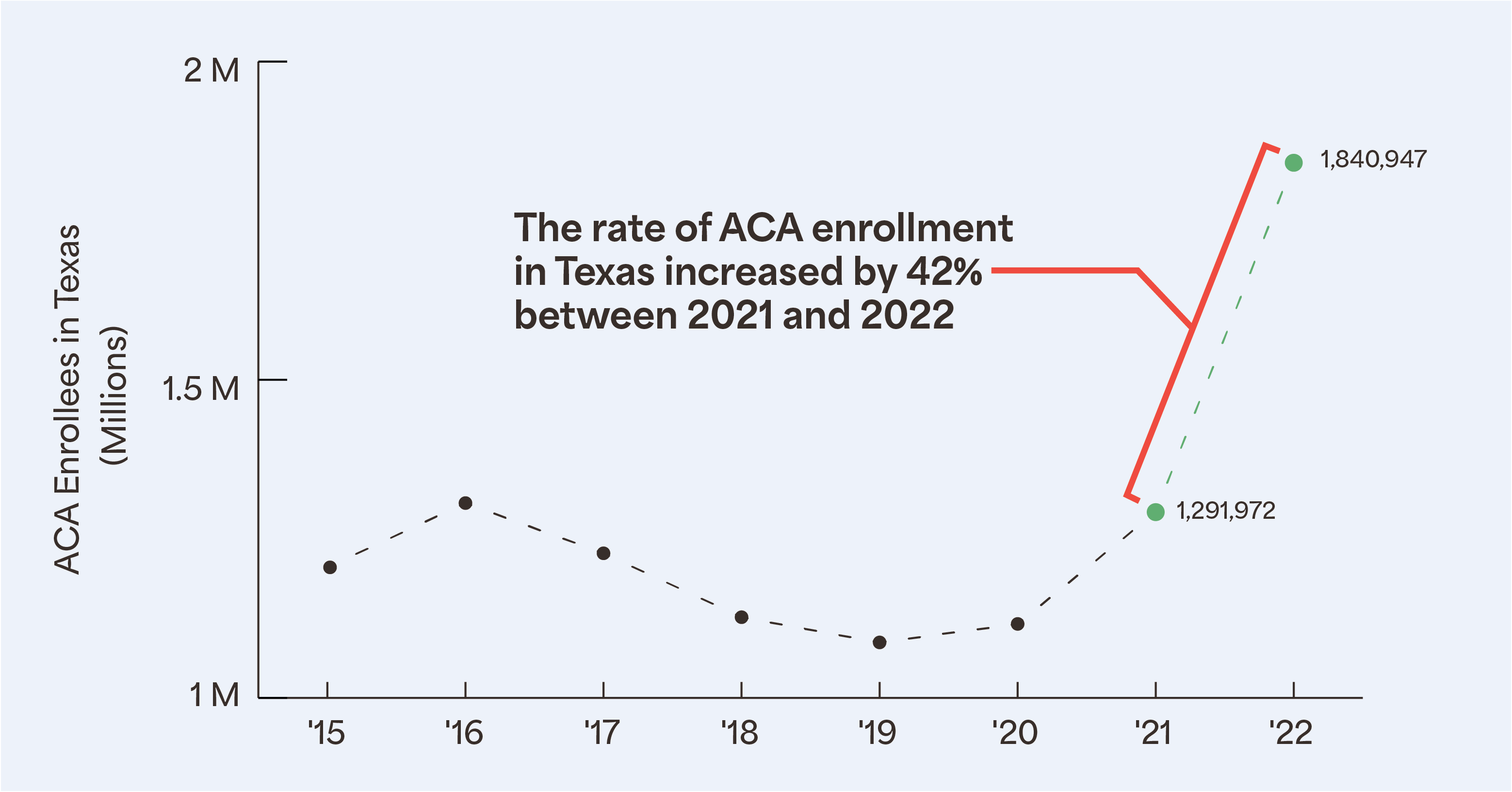
Ideally, the Affordable Care Act (ACA) Marketplace will be a feasible alternative to mitigate the growing uninsured population. The Marketplace offers more coverage opportunities, and therefore greater healthcare access. In 2022, more than 1.8 million Texans enrolled in ACA health insurance, a record for the state. This estimated increase of 500,000 enrollees was likely due to the record amount of federal financial assistance given to pay for monthly premiums. This offers an encouraging outlook for 2023 ACA enrollment, as we can see that there is a great need and value for health insurance in Texas communities.
EHF will continue to work to establish a better health policy environment for Texans to flourish. By sharing our research findings, we seek to generate awareness and conversation about disparate access to health care. Emphasizing the influence of NMDOH on primary care highlights where policy conversations should be oriented for a positive impact on Texans’ health. Our continued polling and data analysis contribute to building the evidence base for investment in primary care access and NMDOH as we work to close the health equity gap in Texas.