
Even before the threat of COVID-19, the health implications of loneliness and social isolation started to garner attention. Social isolation has been linked with adverse health issues such as depression, poor sleep quality, impaired executive function, accelerated cognitive decline, poor cardiovascular function, and impaired immunity.
When the COVID-19 crisis hit, those serious health issues quickly became all too clear.
Early into the response period, when businesses, schools, churches, and many other social gathering locations were closing to reduce the risk of accelerating the spread of the virus, Episcopal Health Foundation joined several funders and higher education institutions to discuss concerns for individuals’ wellbeing as a result of social isolation.
EHF, St. David’s Foundation, Methodist Healthcare Ministries, The University of Texas, and Texas A&M University all joined in these important discussions. The goal was to determine whether there were existing best practices and/or program models to combat loneliness that relied on non-professional staff and/or volunteers and could be replicated or scaled that could be shared with churches and community organizations so they in turn could help congregants, community members, and neighbors who were suffering alone.
The group had conversations with several organizations and churches that provided critical insight into the work of social isolation:
- Cigna
- Interfaith Ministries, Houston
- AARP Foundation
- Texas Health Resource Foundation
- Baker Ripley
- St. James Episcopal Church, Austin
- Calvary Episcopal Church, Bastrop
Additionally, the following sources were essential in the development of the guidelines as they provided context and insight into the need and work being done to address the need.
- Social Isolation and Mortality in US Black and White Men and Women, American Journal of Epidemiology (2019)
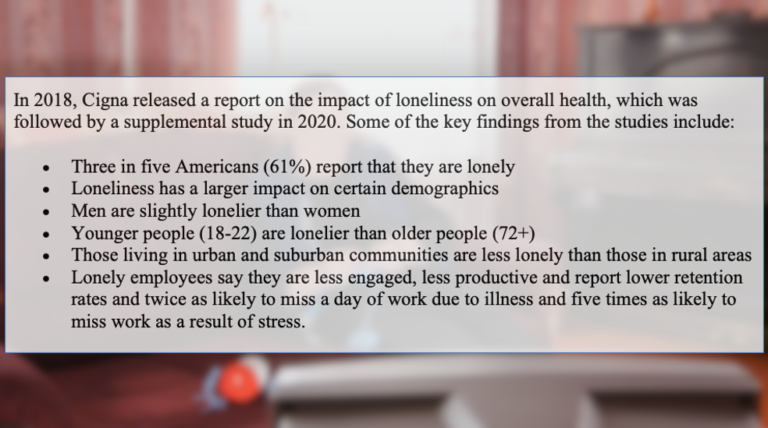
- Cigna U.S. Loneliness Index (2018)
- R U OK? | A Conversation Could Change a Life
- AARP | How to Fight the Social Isolation of Coronavirus
- AARP | Connect2Affect
Researching the effects of social isolation showed a variety of health impacts. An expansive study, conducted in 2019, of more than 580,000 adults found that social isolation increases the risk of premature death for all races for every cause of death. According to the study, social isolation doubled the risk of early death for black participants and increased the risk among white participants by more than 60 percent.
Although these studies are looking at the impact of loneliness on health outcomes in general, what is still unknown is what the overall impact loneliness and social isolation will be on individuals social distancing as a result of COVID-19.
Our discussion group quickly learned that there was no clear understanding of who was doing what in this space. EHF staff researched the landscape, both in terms of issue and geography, to learn more about the work currently being done to address social isolation.
Based on all of the research and disucssions, we identified the following guidelines for organizations that are interested in working to address social isolation:
- Keep it simple. Although conversations were had with groups utilizing technology to improve social connectivity, the pandemic impacted their efforts to fully roll-out their program or to scale it to the emerging increase of social isolation due to physical distancing. However, what has remained effective has been maintaining contact and connection through more traditional means, such as letter writing and telephone calls. Although there is certainly room for technology in curtailing social isolation, simple efforts to make contact seem to be a viable solution for groups seeking an accessible and quick way to reach out to those living alone. Some programs use such simple concepts as a phone call and sitting and visiting to check in on people’s wellbeing.
- Have it be part of something else, not a stand-alone effort. Successful efforts have included those who have incorporated reducing social isolation into the work already being done, such as meals-on-wheels and food pantries. This allows for the use of existing volunteers to keep and maintain contact with a group’s existing client base.
- Work within trusted networks/systems. As one would imagine, concerns about predatory efforts to take advantage of those most vulnerable are always valid and perhaps even more heightened today. Groups such as AARP, Meals-on-Wheels, and Cigna Medicare Advantage are capitalizing their role as trusted resources to ensure their members are not suffering from social isolation. If efforts to reduce social isolation can be joined with the efforts of a trusted partner, such as a church making its volunteer base available to Meals-on-Wheels to make phone calls, legitimacy is gained, and trust is easier to establish.
- Employ an easy approach to training. Because models that utilize more complex tools and resources might require significant training of volunteers, or clients if the model is tech-heavy, training can be quite involved. However, by not over-complicating training and utilizing simple scripts for conversational prompts it is easier to establish parameters for volunteers, allows for them to be engaged quicker, and is a good reminder that the actual purpose is a very basic one: to provide interpersonal contact.
- Work within an existing model. By replicating what others are doing, you are able to learn from their experiences about what has worked, what has not, and what challenges you might anticipate. Further, by doing so, there is the added benefit of utilizing existing scripts and training material developed for a particular model.
- Use existing resources, refocused. Utilizing existing volunteers who are already familiar with you, and you with them, some groups have been able to redeploy resources in a way that reduces social isolation. In some cases, volunteers for programs, such as a senior nutrition center, that have been sidelined due to the COVID-19 have been used to provide social contact with individuals living alone. Similarly, Cigna has redeployed its outbound sales staff to provide outreach and make phone calls to individuals at risk because they live alone and may have underlying health concerns.
As many people are following social distancing protocols, the potential harm due to social isolation must be considered, especially during a prolonged period. Care must be given to, as one EHF staff person said, “to focus on distancing PHYSICALLY and not distancing SOCIALLY.”
What is key for any effort to reduce social isolation and loneliness is to remember to place the focus on providing a human connection, perhaps even developing companionship, instead of feeling the need to fix issues. However, if an issue is brought to light, volunteers must have referral resources that can help follow up and address a concern. Nevertheless, it is critical to remember that the fundamental aspect of any effort to reduce social isolation is simple human contact.
