
What We Believe
EHF’S CORE VALUES:
- Informed Action
- Collaboration
- Empowerment
- Stewardship
- Transparency
- Accountability
- Transformation of human lives and organizations
- Compassion for the poor and powerless
Our Values and Principles
As an instrumentality of the Episcopal Diocese of Texas, we are grounded in our gospel commitment to know and serve our neighbors. This plan is grounded in our core values, which were developed by our board when the foundation was created.
In addition, we rely on health equity as a central guiding principle that directs our approach.
As a health foundation aligned with public health principles, we have a deep commitment to health equity and to reducing the barriers that prevent individuals and communities from reaching their full potential. We view all of our potential investments through a health equity lens. There are many definitions of equity, but we return to the World Health Organization’s (WHO) explanation frequently and share it here as important context:
Equity is the absence of avoidable, unfair, or remediable differences among groups of people, whether those groups are defined socially, economically, demographically or geographically or by other means of stratification. ’Health equity’ or ’equity in health’ implies that ideally everyone should have a fair opportunity to attain their full health potential and that no one should be disadvantaged from achieving this potential.
For the Episcopal Health Foundation, this means we seek out opportunities to level the playing field so that vulnerable populations have the same chance of achieving good health as other groups. We consider vulnerable populations to include members of groups that lack full opportunity to participate in and benefit from the health system, often due to poverty, discrimination, immigration status, insurance status, or disability.
On the ground, our commitment to equity means that we are taking deliberate action to improve the health of vulnerable communities. As a Christian organization, we take seriously Jesus’ teaching about caring for the poor and marginalized. In the context of health and healthcare in modern day Texas, this translates to working for the benefit of low-income and vulnerable populations.
What We’ve Learned
When we released our first plan, we outlined three goals and seven strategies to scope our work. Our intent was and is to go deep and not wide – to invest in multiple ways that could support transformation to healthy communities throughout the Episcopal Diocese of Texas. We understood that if we tried to do too many things, we would spread our resources too thin and miss the chance for deeper impact.
After working within the plan for almost three years, we have greater clarity about what our work is, and what it is not. This means we will increase our investment in some areas, and pull back in others. For example, in community engagement, we recognized that we needed to increase our activity in this area to make an impact, so we added staff to work with community partners interested in learning to do effective engagement. In 2017, we actively solicited grant applications and increased our funding for community building work. With respect to grantmaking support for clinical services, we learned that we had spread ourselves too thin. We funded many great organizations doing important work, but the work was so broad-based that we missed opportunities to go deeper and create greater, more lasting impact. The new plan will guide us in making more focused investments so that we will have greater impact over time.
We have learned a great deal that informs our new plan:
The case for change still rings true
Our original plan calling for wholesale transformation was based on the premise that the poor health status of people within our diocese, state, and nation will improve only if the systems and structures that impact health status undergo significant change. Simply put, if we keep doing what we’ve been doing, we’ll keep getting the same results. Changes at the margins will bring only marginal improvements.
The United States spends $3.2 trillion a year on health and over $40 billion at the state level. This is far more than any other country, and yet our health outcomes are worse than other developed countries, as illustrated in the following graphic. There is nothing inherently wrong with committing almost 20% of our economy to health. What is wrong is that we are not getting value for our investment. The good news is that we have enough money in the health system to improve our outcomes – to help people live fuller, longer lives. The challenge is that we must intentionally aim for improved health outcomes, not simply delivery of more services. This means challenging ourselves to transform the underlying systems and structures so that we get value for our investments in health.

Source: D. Squires and C. Anderson, U.S. Health Care from a Global Perspective: Spending, Use of Services, Prices, and Health in 13 Countries, The Commonwealth Fund, October 2015
We can offer communities more than money
The Episcopal Health Foundation is a multi-faceted entity. While we devote most of our financial resources to grantmaking, we conduct several other programmatic activities in advancement of our goals. We have a research team that conducts and partners with experts to produce original research on important topics such as the impact of the Affordable Care Act (ACA) on uninsured Texans, strategies to optimize rural healthcare infrastructure, and the science of early childhood brain development. The research team created and maintains a web-based data warehouse with mapping tools to help communities understand and use complex health data from multiple sources.
EHF also has teams to support our Episcopal congregations in undertaking transformational outreach work in and with their communities; to teach community organizations how to undertake effective community engagement; and to organize and facilitate health-based community coalitions. We support community-based organizations in building their own capacity by helping them assess their strengths and weaknesses and then underwriting the costs of organizational development. And we have an evaluation team to help us understand and improve the impact of our efforts. Communications ensures that our messages are disseminated publicly and to targeted audiences. Our staff serve on boards, commissions, and committees, and we write, publish, and teach on public health, healthcare delivery, and health policy matters.
We must focus on outcomes rather than interest areas to achieve our goals
We’ve learned that this multi-faceted approach gives us numerous avenues through which to work in communities. In some communities, our congregations have created entry points for community-level work by making introductions and helping us build relationships. This has enabled us to form or join coalitions and to discover grantmaking opportunities we otherwise might have missed. Our research on community clinics’ use of social determinants of health screening tools has led to the development of a learning collaborative among community clinics that receive grant funding to support their work. Not only do our multiple approaches give us a variety of entry points, we’ve recognized that when we deploy more than one tool to a problem or opportunity, our impact multiplies. We will continue to seek out opportunities to amplify impact in this manner.
Looking back at our first three years we realize that our original strategies were not outcome-oriented but were instead descriptions of the areas in which we were interested in working. We had not sufficiently articulated what we hoped to accomplish in each interest area and how they built on each other to accomplish a higher goal. And because we had not articulated desired outcomes, our work was not as focused, deep, or impactful as it might have been. We moved toward greater focus within the first plan by posting guidelines with specified priorities for prospective grant applicants and declining opportunities to participate in good work when it was not tightly aligned with our goals.
Our new plan outlines a scope of work that is grounded in four outcomes that describe the future we want to see. Nine accompanying strategies outline how we will approach that work for the next five years and, we believe, can be leveraged together in powerful ways. While the plan overall might be described as “Strategic Plan 2.0” because we have retained the same vision statement and have largely retained the original three goals, the inclusion of four targeted outcomes creates a sharper focus for our work. This sharpened focus is intended to reflect our calling to support truly transformational change over time. The abundance of resources entrusted to us provide the opportunity and the obligation to do this kind of work.
How We Work
Keeping these values and principles in mind and reflecting on what we have learned so far, we have refined our focus in this strategic plan. We are committed to work that is upstream and systems-focused and that depends on the strength and capacity of community-based clinics as core partners. Here’s what we mean when we say that.
Going Upstream
Our public health orientation leads us to working upstream. This means we are most interested in identifying and preventing the causes of illness and injury.
http://www.countyhealthrankings.org/our-approach
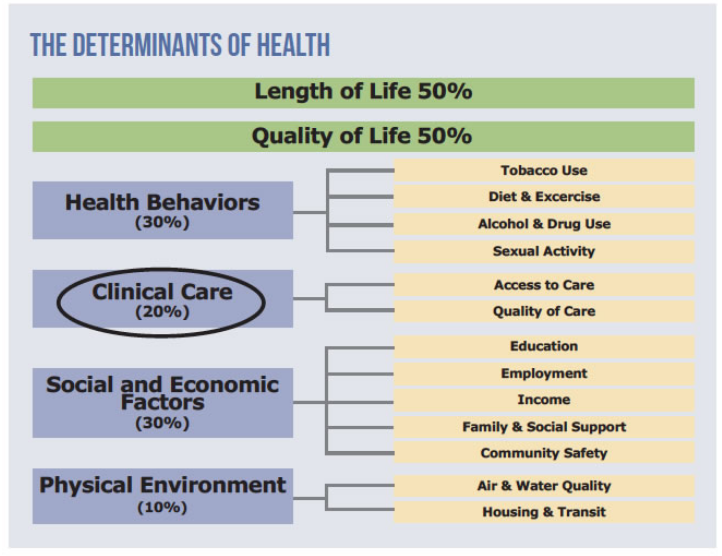
Decades of research have demonstrated that while access to high-quality medical care is essential for population health, clinical care itself makes a relatively small contribution to population health outcomes—likely around 20%. The most influential drivers of health— often referred to as the ‘social determinants of health’—are outside the scope of work of the traditional healthcare delivery system, and include economic, behavioral, and environmental factors. Currently, our health system investments are heavily weighted toward medical care, and are underinvested in addressing the factors that most influence health outcomes. This imbalance is, in part, the result of the great strides made in medicine during the last century to diagnose and treat disease, and is now perpetuated by financing structures that prioritize medical care over other investments in population health. This means we are missing opportunities to improve health outcomes.
The national conversation about value in health expenditures inevitably leads to the question of whether we are spending our health resources in the right places, at the right time. We are encouraged by the interest of health system leaders, payers, community clinics, and many others to advance community health interests by moving up- stream to address the social determinants of health, particularly through community prevention. We look forward to working with partners to move in this direction.
Focusing on Systems
We are most interested in work that takes a systems approach to improving community health. We borrow from the WHO’s definition of a health system as our guidance. WHO describes health systems as: the people, institutions and resources, arranged together in accordance with established policies, to improve the health of the population they serve, while responding to people’s legitimate expectations and protecting them against the cost of ill-health through a variety of activities whose primary intent is to improve health.
This leads us to focus on creating and supporting intentional connections between and among institutions aimed at improving a community’s health. In some communities, health systems are robust and high-functioning, and in others, systems do not exist, are incomplete, or underperforming. We see great opportunity in supporting the development of the networks and financing mechanisms necessary to build and sustain strong health systems.
Additionally, we will shift our work from filling gaps in the health and social safety net to addressing systemic problems that cause and perpetuate gaps. We will seek opportunities to build and improve system-level infrastructure and to support organizations and individuals to make change at this level. This systems orientation supports comprehensive approaches to health challenges rather than ad hoc efforts by independent, sometimes isolated, actors. It also allows us to address ineffective system structures rather than trying to make up for the problems those structures create. It challenges us to move from shorter to longer-term investments and from downstream to upstream interventions.
Partnering with Community-Based Clinics
We believe we can be most successful in our upstream, systems-oriented approach by partnering with community-based clinics. When we refer to community-based clinics we mean healthcare providers (1) that are physically and socially embedded in communities; (2) for whom service to low-income and vulnerable populations is a primary mission; and (3) that provide preventive care, primary care, behavioral health services, and/or oral health services.
These clinics are well-positioned to support the movement of resources upstream toward community prevention. They are part of the healthcare delivery system and part of the community. For the low-income and vulnerable populations served by community-based clinics, the clinic’s ability to affect health system and community-level change is crucial to improving health outcomes. Our work with clinics as key change agents is by no means to the exclusion of other healthcare providers and community partners, but it has been and will remain a central piece of our work.