Nearly half of low-income Texas adults who were disenrolled from Medicaid health insurance after the state began “unwinding” coverage following the height of the pandemic became uninsured. That’s one of the findings of a report by The Harvard T.H. Chan School of Public Health that looked at the impact on Texas and three other states just six months into the unwinding of Medicaid’s continuous enrollment. Episcopal Health Foundation sponsored the report.
“This report gives us an important snapshot of what happens when Texans with low incomes lose affordable health insurance,” says Dr. Ann Barnes, president and CEO of Episcopal Health Foundation. “The results are clear – having health insurance improves engagement in health care activities. Loss of coverage reduces engagement in health care activities. That means fewer ways to prevent disease or get an early diagnosis on a serious condition. The bottom line: being uninsured is a barrier to health.”
As part of the COVID-19 federal Public Health Emergency, Texas paused Medicaid disenrollment in exchange for increased federal funding, allowing Medicaid beneficiaries to remain continuously enrolled without eligibility redeterminations.
Texas began redetermining Medicaid eligibility in April 2023 and the report surveyed Texans with low incomes between September and November 2023, about six months into the unwinding process.
The report looked at the effects of the unwinding process in Texas, Arkansas, Kentucky, and Louisiana.
In Texas, researchers found:
- 15% of Texans who had Medicaid health insurance at some point since March 2020 had been disenrolled.
- Of those who had been disenrolled, nearly half (49%) said they became uninsured.
- 46% of Texans with Medicaid reported moving since March 2020, which is a key risk factor in maintaining continuous insurance coverage.
- 59% who had Medicaid coverage said they had heard little or nothing about the unwinding policy change.
- Of those who had heard about unwinding, 51% had heard about it from media, 34% from a state agency, 27% from a family or friend, 17% from a health insurer, and 15% from a health care provider.
- 61% of Texans say they had heard nothing at all or not very much about the Affordable Care Act health insurance marketplace that may provide options for those who lost Medicaid coverage.
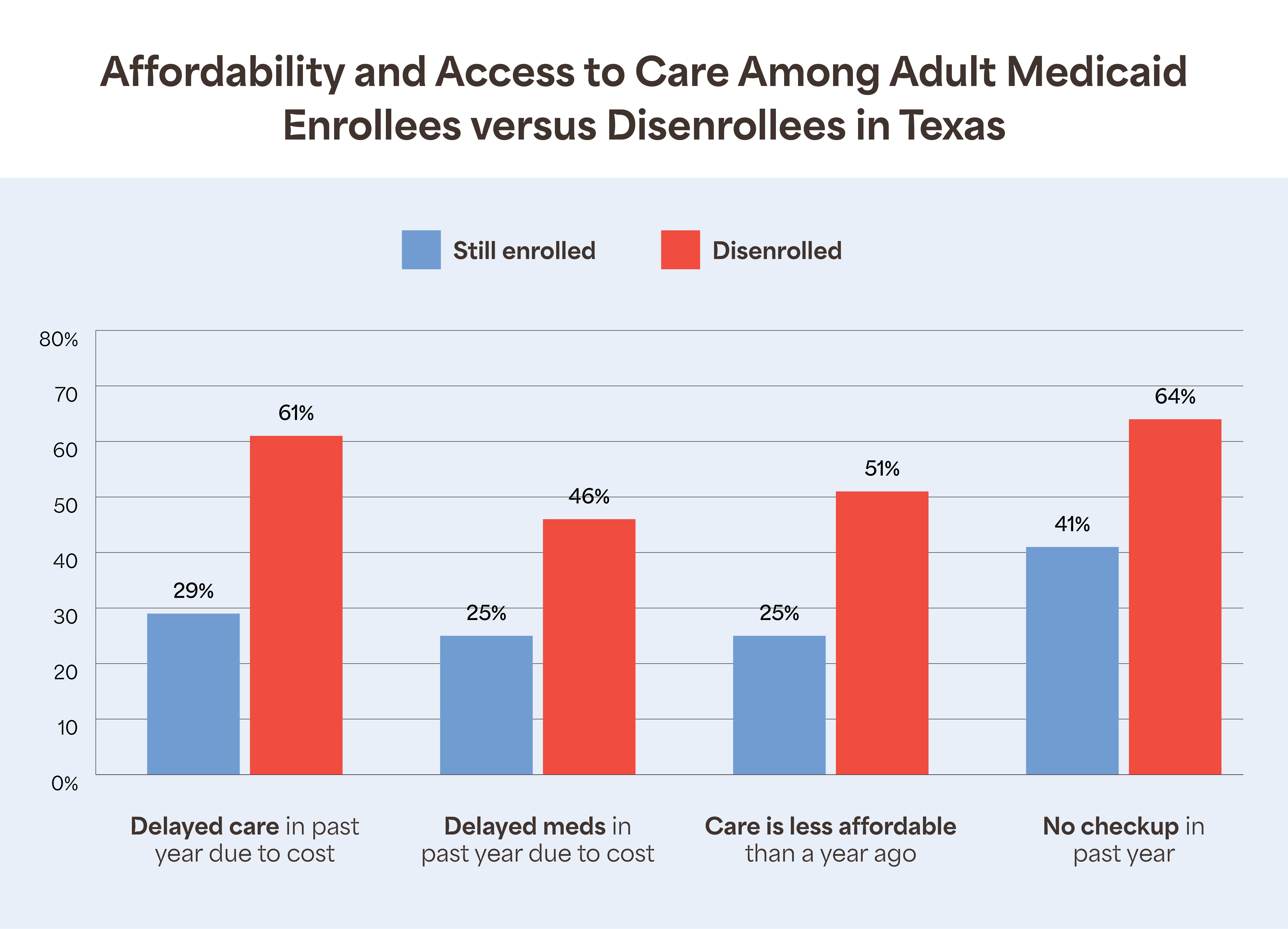
When it comes to how the Medicaid unwinding affected Texans’ ability to afford and access medical care, researchers found that the people who were disenrolled from Medicaid were more likely to report delays in care in the past year due to cost, delays getting medicine, and challenges with affording care.
In addition, nearly two in three disenrolled Texans (64%) reported not having any preventive checkups in the past year.

It’s important to note that the report did not look at how the Medicaid unwinding process affected children across the state. A recent analysis from Georgetown University’s Center for Children and Families shows that by December 2023, more than 1 million fewer Texas children were enrolled in Medicaid or CHIP health insurance following unwinding.
Methodology
Researchers fielded a multimodal survey using random-digit dialing and addressed-based sampling between September and November 2023, just after the unwinding began. They focused on nonelderly adults (19-64 years old) with incomes at or below 138% of the federal poverty level.
The survey included 2,210 respondents, of which 1,471 reported Medicaid enrollment since March 2020. Of the total sample across the four states, 36% were respondents in Texas.