
When Health Affairs published Social Determinants As Public Goods: A New Approach To Financing Key Investments In Healthy Communities in August 2018, it caught our attention.
Foundational to our work at EHF is learning and exploring various social determinants of health (SDOH) financing tools to address community health challenges. The financing model – Collaborative Approach to Public Goods Investment (CAPGI) – explored in this article is especially unique because it benefits multiple perspectives simultaneously, thus presenting a solution to pervasive “free rider” problems that haunts the social-health service eco-system.
We held initial discussions with Dr. Len Nichols, lead author of the article, and ultimately co-funded a national CAPGI learning and feasibility planning initiative with the Commonwealth Fund, Missouri Foundation for Health and California Health Care Foundation.
Based on the initial educational webinars and outcome of the feasibility planning analysis, three sites were selected nationally to pilot the CAPGI model: Waco, TX, Cleveland, OH and Albany, NY. This blog article is written based on EHF’s perspective in supporting the CAPGI pilot in Waco.
In 2020, Prosper Waco started its CAPGI work by engaging organizational partners to understand the mental health service landscape of Waco and McLennan County. Because Prosper Waco operates under a collective impact model, it had experience in identifying local problems through partner discussions. A local FQHC, county mental health department, law enforcement, nonprofit service agency, philanthropy, and local government leaders were all involved in planning and implementing a local social care coordination model as “Waco Connect.” Their approach uses a patient navigator/social service worker model to address the social service needs of community members who have high hospital emergency department usage and frequent touches with the criminal justice system.
Prosper Waco leveraged EHF investments to gain financial commitments from the City of Waco, The Bernard & Audre Rapoport Foundation, and the Baylor Scott and White Health Plan (BSWH) to finance Waco Connect. Simultaneously, EHF contracted with Dr. Len Nichols’ team to provide technical assistance to Prosper Waco and Dr. Laura Dague at Texas A&M University (TAMU) to conduct an independent evaluation of the Waco Connect interventions.
The pilot interventions were completed in 2022 and the evaluation was finalized in 2023.
To learn more, those evaluations can be accessed here:
Waco Connect Project: Health Plan Referrals Evaluation Report
Waco Connect Project: Law Enforcement Evaluation Report
Based on our experiences and the evaluation reports, we would like to offer some reflections:
Both evaluation reports offer some short-term promising results
With the police department intervention, TAMU researchers found that the implementation of new procedures, developed in collaboration with the social resource coordinator (SRC), resulted in a reduced need for police officer intervention in response to behavioral health calls. By saving valuable officer time, the value of the intervention was immediately obvious to Waco Police Department, which quickly implemented these procedures for all shifts. This intervention’s significance was so valuable that the Waco Police Department hired the SRC from Prosper Waco.
However, the researchers cannot evaluate impacts on individuals detained or involved in the calls. Despite this, it is reasonable to infer that their time for treatment would have decreased, and they were more likely to receive medical screenings and psychological evaluations.
In the intervention funded by the BSW Health Plan between April 2021 and February 2023, the SRC successfully contacted 291 BSWH Medicaid members and identified social needs for 232 clients. WC clients identified the following needs in which they wanted assistance: housing (143 clients); utilities (131 clients); food (79 clients); and childcare (60 clients). To understand if this assistance resulted in a reduction of health care costs, the researchers compared the health outcomes of the WC clients to those of a matched control group from BSWH’s Medicaid plan. While they found no evidence of reduced health care cost of care, they did find some evidence of reductions in the number of emergency department visits following Waco Connect referrals.
COVID-19 pandemic impacted Waco Connect
At the start of the planning process, Prosper Waco engaged four types of stakeholders: health plans, hospitals, law enforcement, and local philanthropy. However, the unexpected COVID-19 pandemic caused delays in these conversations and altered stakeholder interactions from face-to-face to virtual. Nonetheless, building on its longstanding track record as a collective impact backbone, Prosper Waco was able to secure financial commitment from BSWH, the City of Waco Police Department and the Waco Foundation. Citing COVID-related revenue losses, the two main local hospitals elected not to participate financially. In our opinion, the lack of hospital engagement did not help to secure broad payer support for the work.
Translating an economic model on SDOH financing into practice was challenging
During the planning phase, EHF staff had worked closely with Dr. Nichols to educate Waco stakeholders about the critical importance of “trusted broker organization” in facilitating of the negotiation of pricing between the payers and providers of social care. However, the technial assistance team noted that Prosper Waco deviated from the model requirement of being a “trusted broker” when selecting an organization to implement the model. Instead, it pursued a traditional fundraising approach, securing grants from BSWH, Waco Police Department and local philanthropies to implement the Waco Connect social service activities.
Prosper Waco became the trusted broker and the social care provider, which undermined the broker’s impartial role in negotiating costs. As a result, the CAPGI model—as laid out by Dr. Nichols–was not fully implemented.
Project staff turnover challenged Prosper Waco and its Partners
During implementation, several CAPGI champions retired. In the middle of the intervention, there was turnover in the project manager position and in the BSWH staff position leading the Waco Connect project. “Change management” was a constant theme as both EHF and the TA team needed to reorient new leaders and staff involved in the project.
Losing momentum due to delay in securing evaluation data
Staff turnover at both Prosper Waco and BSWH, coupled with the messiness of the implementation, resulted in extended delays for the TAMU research team to access the BSWH health care utilization data. By the time the evaluation findings became available, the pilot had ended and many of the program designers and implementers had departed. There were no opportunities to inform or refine the intervention based on the evaluation data.
EHF'S Key Takeaways
As we share our reflections of this work, our intent is not to point fingers or lay blame. EHF and the TA and evaluation teams shoulder shared responsibility for not seeing, reacting and adapting to the emerging challenges. As a health philanthropy, we need to document the critical learnings here as well as to apply these lessons for our future investments, especially considering EHF’s new strategic framework.
Despite these challenges, we agree with the TA and evaluation teams: if extended to a longer period and with staffing stability within Prosper Waco, we would likely see different outcomes. Equally important, let’s not overlook the two important short-term outcomes of “social care coordination” interventions: less police time spent on behavioral health calls and evidence of reductions in the number of emergency department visits following Waco Connect referral calls. Both are promising outcomes from the Waco Connect pilot project.
From a sustainability perspective, we are pleased to share that the Waco Police Department has hired the Prosper Waco SRC as a permanent addition to its staff. BSWH is continuing to support a similar Waco Connect model with Goodwill Industries in Waco. Despite not adhering to the CAPGI model fidelity, one can argue that the work is successful in getting payers to fund social care coordination in addressing complex community health challenges.
Most importantly, the evaluation findings in the Waco Connect pilot will add to important evidence based of SDOH interventions in Texas as Texas Health and Human Services Commission (HHSC) is in the midst of developing and implementing strategies through its Non-Medical Drivers of Health Action Plan as well as implementing HB 1575, a bill that was passed in the 2023 legislative session to expand reimbursable provider type to include community health workers and doulas under HHSC’s Children and Pregnant Women program. ⚙
More from Digging Deeper

Texas’ Medicaid Managed Care Learning Collaborative: Origin, Contexts, and Key Takeaways from 2024 Efforts
Episcopal Health Foundation (EHF) launched a partnership with key stakeholders more than six years ago to harness the capacity of MCOs in addressing non-medical needs of Medicaid members. The Learning Collaborative’s work has contributed to key legislation and policy changes that advance the NMDOH work of Medicaid MCOs to continually
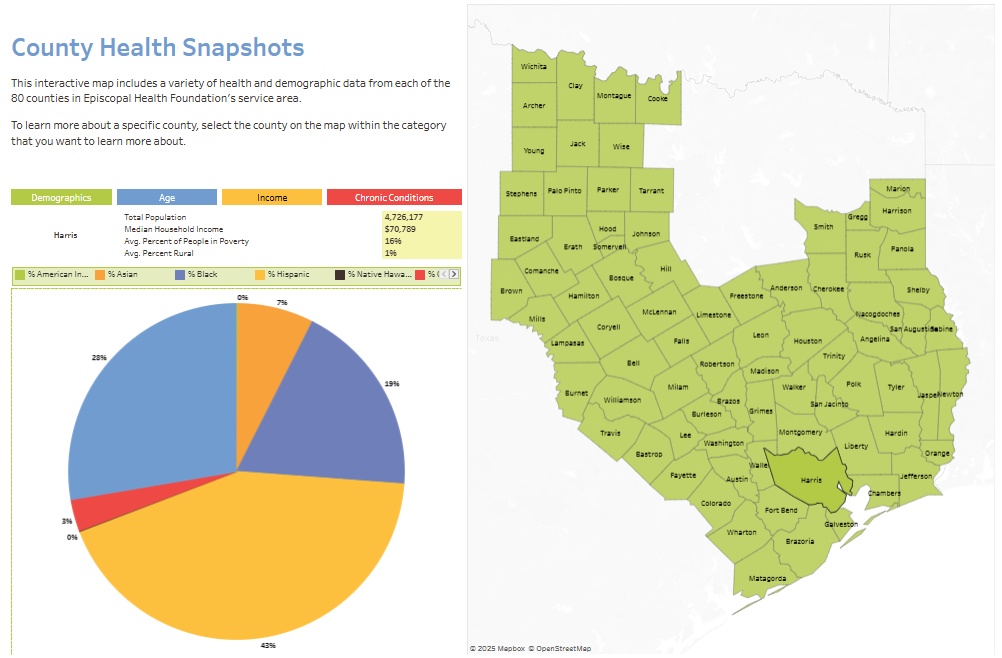
Understanding Community Health Through Data Mapping
EHF’s research team has released an updated and improved County Health Snapshots data mapping tool. EHF’s County Health Snapshots (CHS) tool provides a peek into the important demographic factors and health outcomes within the EDOT.
Key Takeaways from EHF’s Policy and Research Reports in 2024
As a major health philanthropy in Texas, EHF has developed a diverse range of tools, both financial and non-financial, that help to improve the health of all Texans.