
By Shao-Chee Sim
VP for Research and Evaluation
Behind the daily deluge of charts and data about COVID-19 cases and hospitalizations, we are seeing the growing importance of non-medical factors, or social determinants of health (SDOH), in understanding how best to craft public policy responses to the pandemic. These social factors, such as race, income, housing, education factors, and more have been exacerbated by COVID-19 and contribute to health inequities during the pandemic.
We anticipate the increased focus on SDOH will only add to recent federal and state policy initiatives that incent greater health care investments in SDOH. For example, Centers for Medicare & Medicaid Innovation awarded $155 million to 30 communities for the Accountable Health Communities (AHC) model in 2017, a five-year project that supports local communities in addressing the health-related SDOH needs of Medicare and Medicaid beneficiaries. Out of the 30 sites selected, three sites are based in Texas. In 2019, EHF and Robert Wood Johnson Foundation are sponsoring a learning collaborative for the Texas Medicaid agency and its managed care organizations to strengthen the capacity of these organizations in developing and implementing SDOH strategies.
While there is increased policy momentum to strengthen the role of health care systems in identifying and addressing patients’ SDOH needs, the language of SDOH is not fully understood and often misinterpreted, especially among health care consumers.
So, what is SDOH?
At its core, SDOH refers to the notion that health is shaped by many factors beyond medical care. According to World Health Organization, SDOH is defined as the “conditions in which people are born, grow, work, live and age….” Healthy People 2020 defines SDOH in five inter-related domains: economic stability, education, social and community context, health and health care, and neighborhood and built environment. While some may tend to interpret SDOH from a “deficit” frame, it is equally important SDOH can also be framed as “asset-based” or protective factor of good health.
Because we understand the importance of consumers’ understanding of SDOH, EHF commissioned the first-ever Texas public opinion survey on SDOH. The survey revealed that the majority of Texans understand that having good medical care is not enough for a person to live a healthy life. They also believe Texans would be healthier if the state government, health insurance, and doctors address these underlying, non-medical factors that affect health.
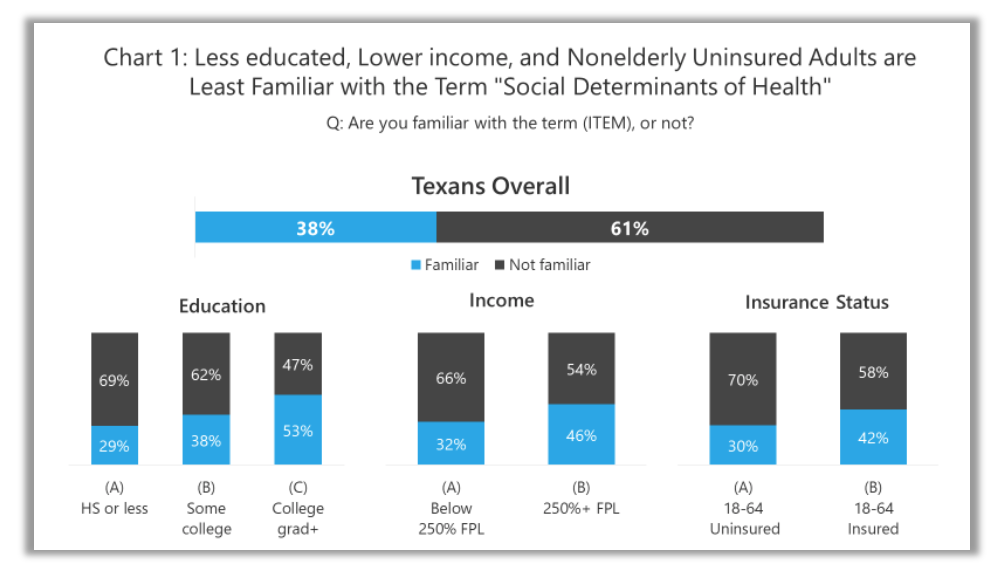
While the survey shows a basic knowledge and appreciation of the value of SDOH, the terminology used by those in the field is not well understood by the public.
 Note: Don’t know/Refused responses are not shown
Note: Don’t know/Refused responses are not shown
When asked if they are familiar with the term “social determinants of health,” fewer than four in 10 (38%) say they are familiar with the term, but six in 10 (61%) say they are unfamiliar (see chart above). Those who are least familiar with the term “social determinants of health” are those with less education (29% High School or less), those with lower incomes (32% below 250% Federal Poverty Level), or those with no health insurance coverage (30%).
We also asked survey participants about their familiarity with other terms or phrases similar to SDOH. The survey responses show that just one-third (33%) are familiar with the phrase “drivers of health” and slightly fewer (29%) are familiar with the phrase “upstream causes of health.” A larger portion of the Texas adult population is familiar with the term “non-medical factors” (56%) and even more are familiar with the phrase “social risk factors” (60%).
As SDOH work continues to grow nationally and in Texas, there is an opportunity for public and private funders, health system leaders, social service providers and other stakeholders to develop consensus in the use of SDOH terminology. We should avoid projecting “negative” or “deficit” connotations when communicating about SDOH to various stakeholders.
The pandemic has created important opportunities for public dialogue and policy discussion about ways to address SDOH challenges. It is never too late to figure out how best to educate health care consumers, especially those with the least resources, about SDOH terminology.
