The Basics of Medicaid Expansion
Medicaid Expansion is a provision of the Affordable Care Act (ACA or Obamacare) that called for state expansion of Medicaid in order to provide health insurance to cover more low-income people. As part of the expansion, Medicaid eligibility would be extended to adults up to age 64 with household incomes under 138% of the federal poverty level — $18,000 for individuals, $24,000 for couples, and $37,000 for families of four.
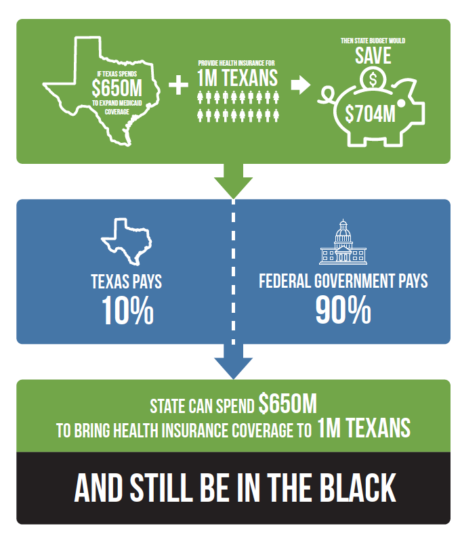
Funding to pay for these new Medicaid enrollees was covered by the federal government under the ACA and gradually decreased to 90% in 2020, with the states paying for the remaining 10% of the costs. However, in June 2012, the Supreme Court ruled that states could not be forced to expand their Medicaid programs, which led to some states opting in and others choosing not to expand.
Texas Doesn’t Expand Medicaid
Texas is one of 12 states that decided not to opt into Medicaid expansion and that decision left more than 1 million low-income Texans without the option for affordable health insurance. That’s because the state’s decision not to expand Medicaid created a coverage gap for 1.4 million Texans who made too much to qualify for Medicaid, but not enough to qualify for subsidies under the ACA. (In Texas, adults who are not pregnant, blind, or disabled generally do not qualify for Medicaid). These people would have been covered by Medicaid Expansion.
What Does This Mean for My Community?
Many congregations across the diocese are ministering to families and communities devastated by COVID-19. They have lost their jobs and their health insurance or they are struggling to work in front-line jobs without health insurance. Others had underlying pre-existing chronic conditions before COVID-19 due to a variety of community and socioeconomic issues, including lack of health insurance and access to affordable medical care. Many of these Texans would be covered under Medicaid Expansion.
“The rise in the number of uninsured in Texas from COVID-19 job losses has led many in the general population to think more about the value of health insurance,” says Elena Marks, EHF’s president and CEO.
“I’m hoping that it’ll persuade legislators to understand that for a substantial group of people, Medicaid Expansion is the only solution, and that it’s actually affordable to the state more so than leaving these people uninsured,” says Marks said in an interview with Spectrum News 1 Texas.
EHF has sponsored several evidence-based, data-driven reports on the impacts of Medicaid Expansion in Texas
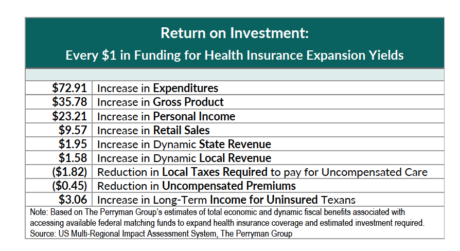
The latest report from the Perryman Group says Texas could provide health insurance coverage using Medicaid federal funds and “reap notable economic and fiscal gains in the process.”
Another report sponsored by EHF shows that while Medicaid Expansion would initially cost the state $650 million, it would then save Texas more than $700 million per year and provide health insurance coverage to more than 1 million Texans. The report found the savings would come from offsetting existing costs for current Medicaid, state health programs, and additional revenue. Opting out of Medicaid Expansion means that Texans are not accessing funds intended for the more than 1 million persons who qualify.
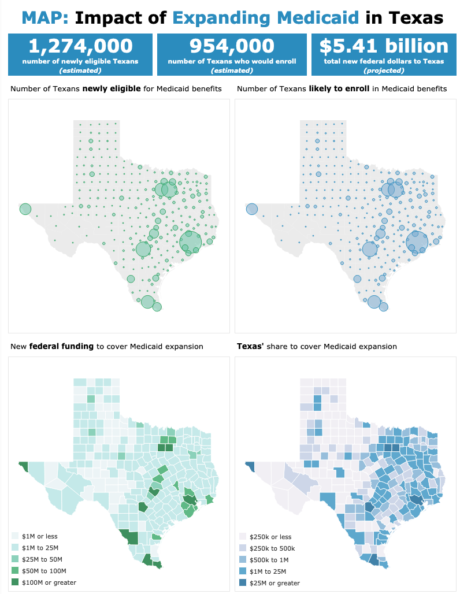
Another EHF-sponsored study found that more than 950,000 newly-eligible adults would enroll in health insurance under Medicaid Expansion in Texas, bringing a projected $5.4 billion in federal dollars to the state. The new study was written by Laura Dague and Constance Hughes at the Bush School of Government & Public Service at Texas A&M University.
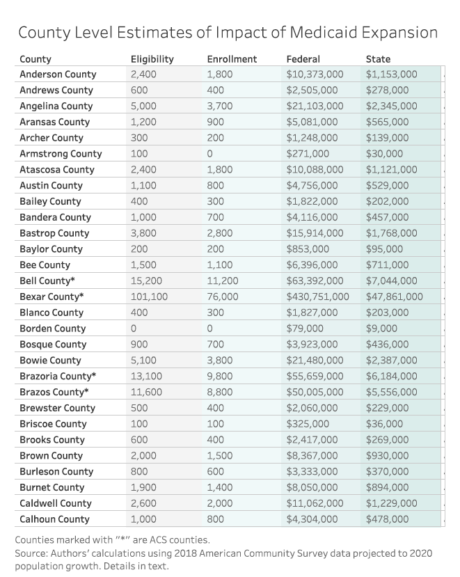
Click on the map and/or table below to see the impact of Medicaid Expansion in your county, including the number of people eligible for Medicaid Expansion, as well as how much new federal annual Medicaid spending would be expected: