In 2025, Episcopal Health Foundation continued to focus on improving health, not just health care for all Texans.
That meant publishing research to highlight what’s working, elevating Texans’ voices through statewide polls, and sharing practical findings that policymakers, health plans, clinics, and community partners can use.
Here are the big takeaways from the major EHF reports and roundups we posted this year:
- Prevention matters. Scale diabetes risk screening and evidence-based prevention, prioritize maternal risk identification and postpartum supports, and expand Non-emergency Medical Transportation (NEMT) use through easier processes and better messaging.
- Keep care affordable. Protect health insurance coverage gains, maintain affordability support, and tackle the non-medical drivers that raise health risks and costs.
- Use data carefully. Pair statewide rankings and model outputs with local data and lived experience; choose measures that drive real action, not just scores.
- Align systems. Strengthen ties among health insurance plans, public health entities, community providers, and social care organizations to finance outcomes across medical and non-medical services.
Select Findings from 2025 Policy Research Reports
Texans are still struggling with affordability and are skipping care because of cost
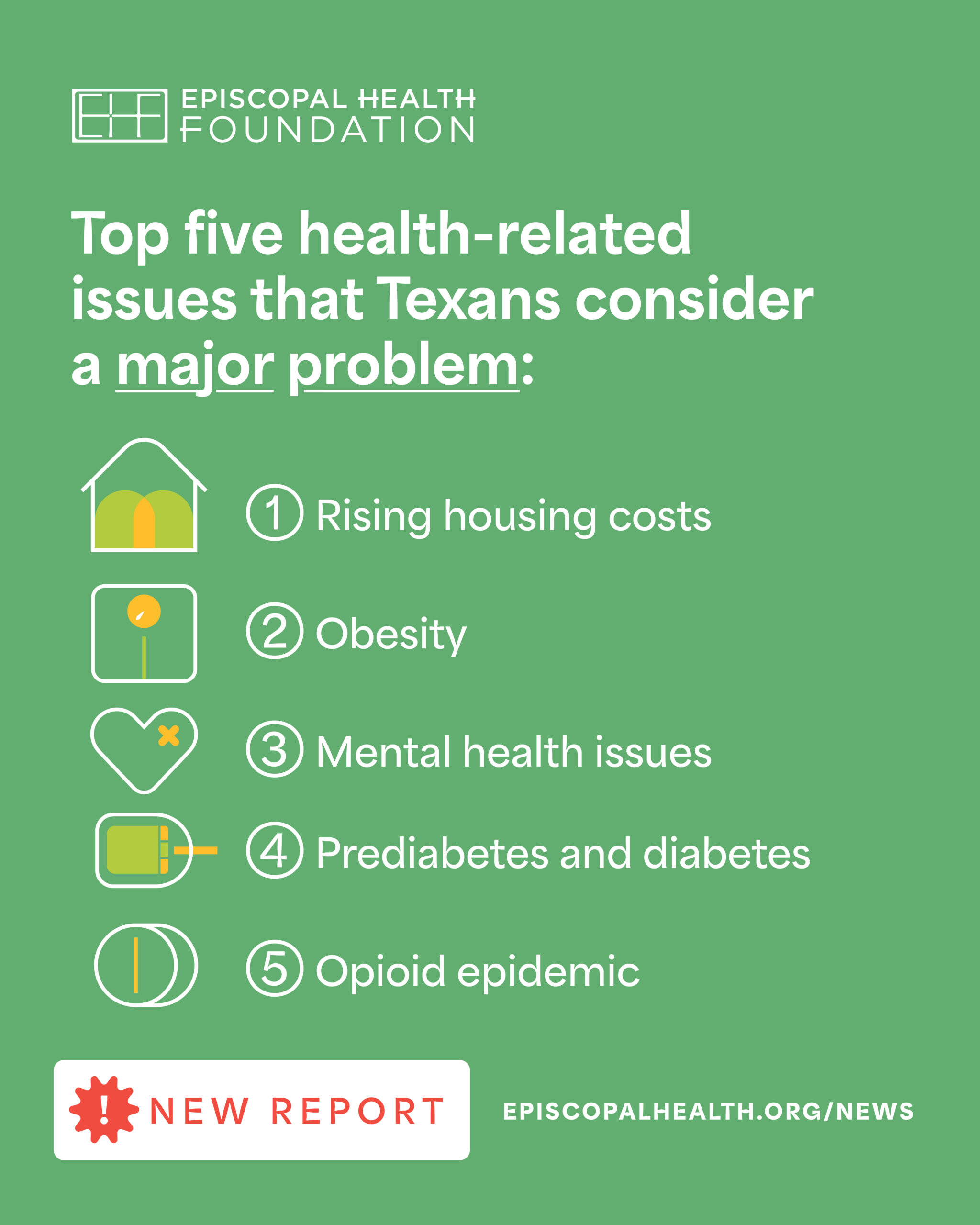
EHF’s annual Health Tracking Poll showed what many families experience: rising costs make it hard to afford care, and people are putting off needed health services.
Nearly two thirds of Texans reported skipping or postponing care in the past year due to cost; almost half said it’s difficult to afford health care; and many named diabetes and obesity as top health concerns. Many also believe the state can do more to help low-income residents with accessing care.
Health insurance coverage dynamics: changes to enhanced federal subsidies could raise the number of uninsured Texans; ACA marketplace affordability matters
Several health policy research papers looked at health insurance coverage issues. One analysis projected uninsurance increases in Texas if enhanced federal Affordable Care Act (ACA) marketplace subsidies ended, and another examined Texans’ experiences when affordability protections lapse, bringing members’ voices into policy conversations about cost and continuity.
These reports emphasize why affordability matters and how sudden policy shifts can disrupt health coverage.
Transportation remains a barrier and Medicaid’s NEMT benefit is underused
We took a deep dive into the state’s Medicaid Non-emergency Medical Transportation (NEMT) benefit. Overall, NEMT is a powerful tool to help people get to needed appointments, pharmacies, and services, but many eligible Texans aren’t using it. The report breaks down how NEMT works, where utilization lags, and practical fixes — including clearer communication and easier scheduling to better coordination among health insurance plans and brokers.
Maternal health: high-risk pregnancies are common and more costly, and postpartum behavioral health needs are under-treated
EHF commissioned Milliman, Inc. to analyze high-risk pregnancies within Texas Medicaid. They found that more than 35% of pregnancies in STAR (the Medicaid program covering low-income children, pregnant women, and families) were high-risk in 2021 and that these pregnancies were roughly 1.3 times more costly than non-high-risk pregnancies. Postpartum behavioral health needs are significant, yet service use is low.
The report points to prevention, better risk identification, and improved postpartum support as high impact steps.
February 26, 2025
We discussed these high-risk pregnancy findings with health insurance plans at our MCO NMDOH Learning Collaborative in April 2025. Plans highlighted the importance of 12-month postpartum Medicaid health insurance coverage and the roles that doulas and community health workers can play in case management and member engagement.
Diabetes prevention: a crucial need for Texas — clinically, financially, and operationally
Milliman’s analyses and literature reviews in 2024–2025 quantified the cost of diabetes to Texas Medicaid was an estimated $6–$8 billion annually. The data summarized what works best in Diabetes Prevention Programs.
The takeaway is simple: prevention and early detection can avert many diabetes cases and save substantial money If programs are implemented at scale and with attention to access and equity.
Using technology and data wisely: pros and cons for AI and rankings
This strategy paper explores integrating health AI in safety-net and rural settings. Better triage and smarter workflows are possible, but success depends on local capacity, data quality, and guardrails to ensure equity, privacy, and safety.
We also published an assessment of the County Health Rankings & Roadmaps framework. It’s widely used and helpful for communication, but rankings may lack reliability, especially in rural areas with small samples or limited data.
The message: use rankings as a starting point, supplement with local data, and focus on actionable indicators.
As shared in this feature by Grantmakers in Health, EHF and partners helped advance several policies that take important steps in addressing diabetes, food and nutrition support, and maternal health through Medicaid during the 2025 Texas legislative session.
EHF shared major economic cost reports relating to diabetes and high-risk pregnancies with legislators and these reports were cited in many committee hearings. The reports underscore how prevention and targeted supports can improve health while saving the state money.
If there’s a single theme from 2025, it’s that affordability, prevention, and practical support (like transportation, food, and postpartum care) must work together to improve health.
More from Digging Deeper
2025 Digging Deeper Digest: A Year Framed by Data, Partnership, and Policy
Spotlighting systems, policies, and partnerships that shape the health of Texans

Transforming Rural Health in Texas: How Strategic Alignment Drives Lasting Change
The HHSC Rural Health Transformation Fund application is a comprehensive, forward-looking blueprint for rural health in Texas. If funded and implemented, Rural Texas Strong has the potential to transform rural health systems, reduce health disparities, and ensure that every rural Texan has a better opportunity to live a healthier life.
Four Ways to Use County Health Rankings and Roadmaps
Key Insights & Recommendations for Public Health Leaders and Policymakers When Using the County Health Rankings & Roadmaps