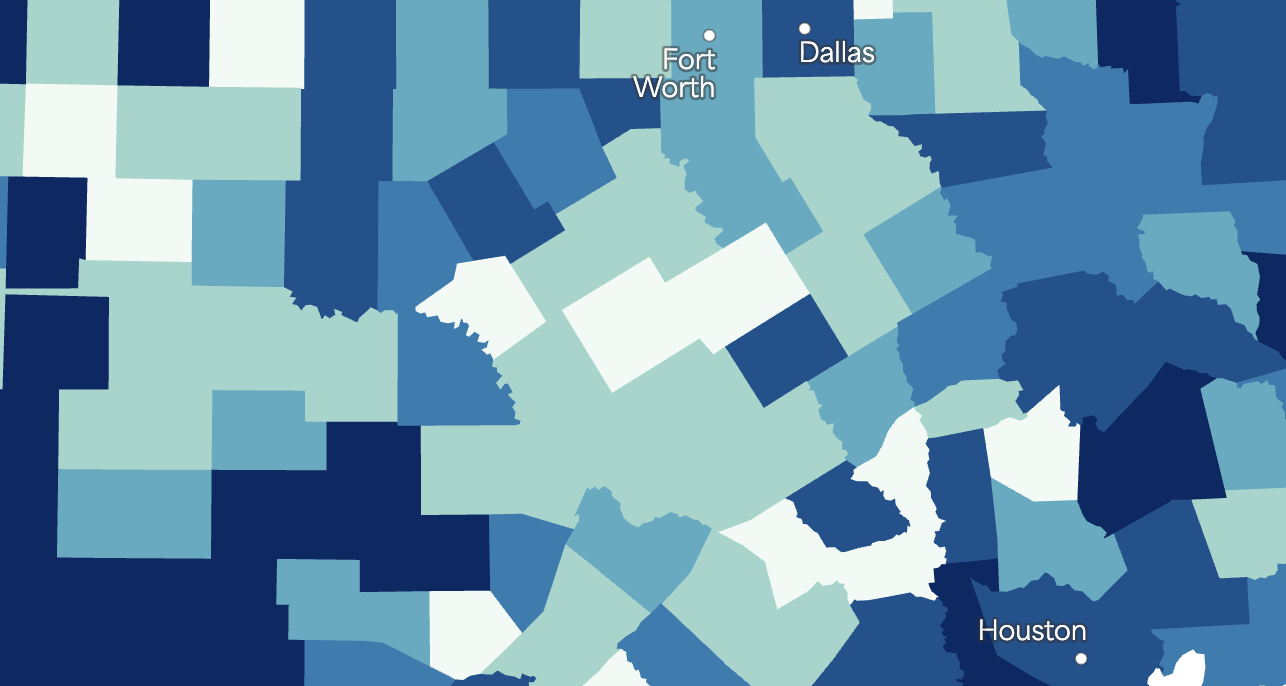
Episcopal Health Foundation collaborated with Treat Oaks Strategies and a Harris County-based marketplace health insurer, to elevate the voices of marketplace members amidst the anticipated expiration of the enhanced ACA Marketplace premium subsidies. The findings from our focus groups and supporting data reveal a complex landscape for Texans relying on ACA marketplace coverage, especially in the face of potential subsidy expiration. Three central themes emerge: the centrality of affordability and continuity of care, the vulnerability of specific populations, and the evolving role of Federally Qualified Health Centers (FQHCs) as a safety net.
Theme 1: Affordability
Affordability emerged as a central concern for marketplace members when selecting and maintaining health coverage. While some participants initially found ACA plans to be reasonably priced, many reported that rising premiums have pushed coverage to the edge of unaffordability. The anticipated expiration of enhanced premium subsidies has amplified these worries, with nearly all focus group participants expressing fear that they would be unable to maintain coverage without continued financial assistance. Several individuals described making difficult choices between health insurance and other essential expenses, highlighting the precarious balance many Texans face in managing their health care costs.
Theme 2: Continuity of Care:
Continuity of care was another top priority for participants, influencing their decisions about which plans to choose and whether to remain enrolled. Many individuals emphasized the importance of maintaining relationships with their existing providers and ensuring access to necessary specialists without additional barriers, such as referrals. Concerns about disruptions in care, whether due to changes in provider networks, formulary restrictions, or unaffordable premiums, were frequently cited. Participants shared that continuity of care not only affects their health outcomes but also their overall sense of security and stability in managing ongoing health needs.
Theme 3: Impact on Vulnerable Populations:
The analysis underscores that the potential expiration of enhanced subsidies would disproportionately affect Texans with lower incomes and those managing chronic health conditions. Participants’ stories highlight the real-world consequences: some would be forced to forgo care, others would attempt to find lower-tier plans with reduced benefits, and many would face difficult choices between health care and other necessities. The anticipated premium increases could create additional barriers to timely, continuous care for those who need it most.
Theme 4: Safety Net Implications:
The potential expiration of enhanced ACA premium subsidies could significantly increase demand on Texas’s health care safety net. Federally Qualified Health Centers, which provide essential primary care regardless of ability to pay, serve as a key component of that system. Focus group responses suggest that while FQHCs are viewed as a critical resource, participants have varied levels of familiarity and expectations. Participants recognized their value but noted challenges such as wait times and continuity of care, while others assumed they could easily access services. If marketplace coverage becomes unaffordable, FQHCs and other safety net providers may face heightened strain, with implications for timely access and system capacity across the state.